c reactive protein rheumatoid arthritis
:max_bytes(150000):strip_icc()/188021_color3-5be479cdc9e77c0051389c14.png) C-Reactive Protein Test: Uses, Side Effects, Procedure, Results
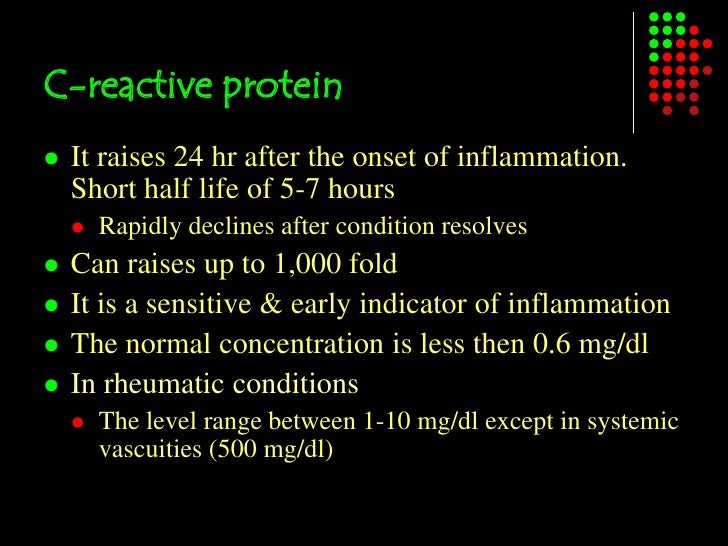
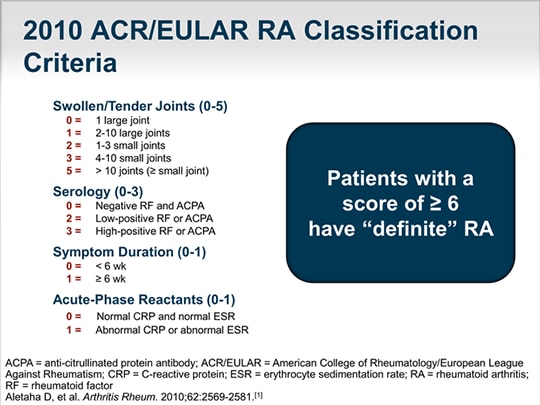
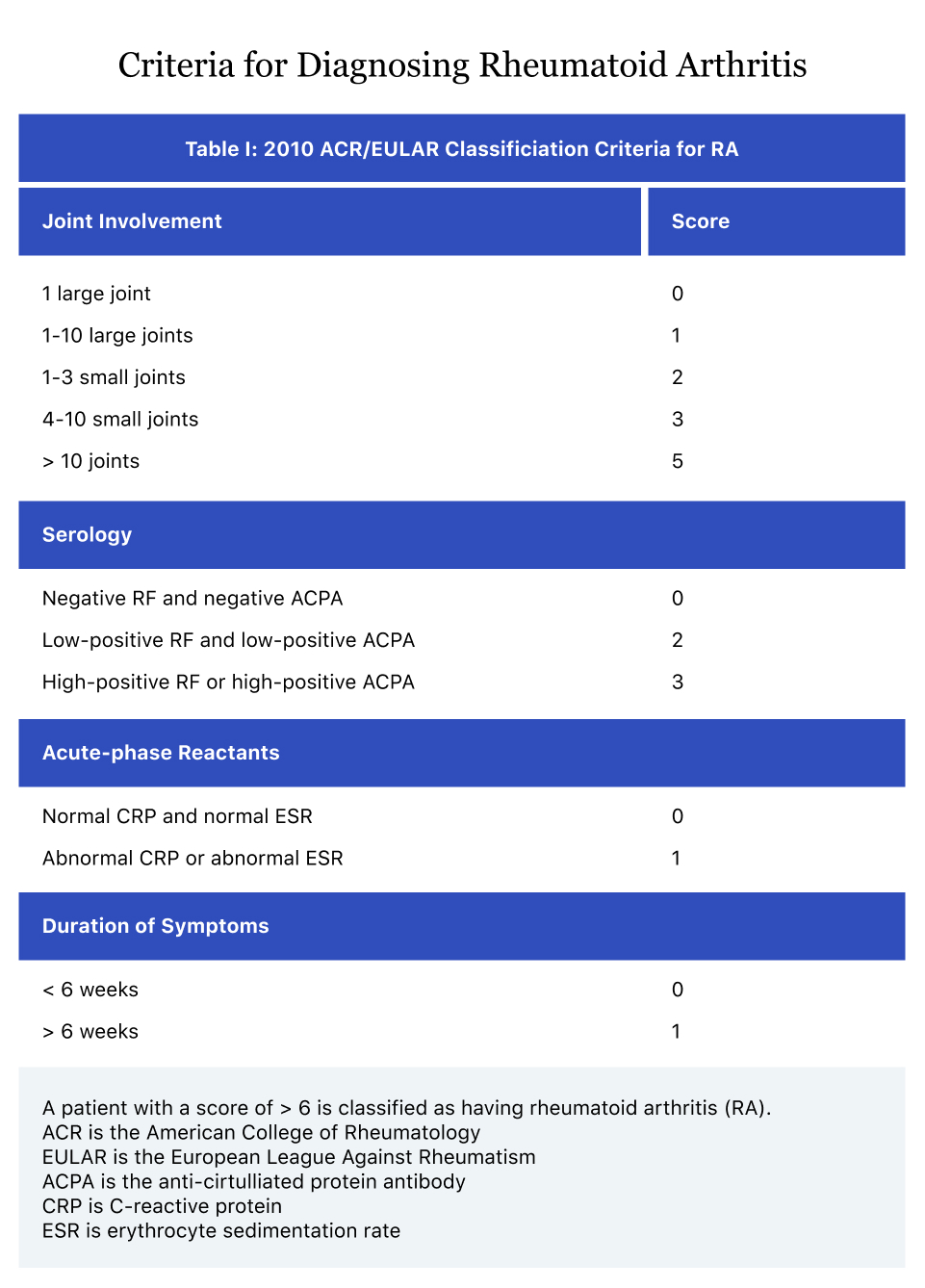
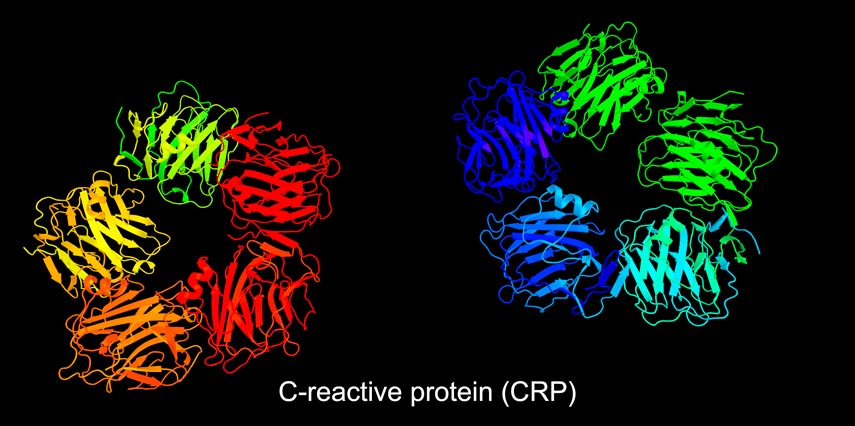
C-Reactive Protein Test: Uses, Side Effects, Procedure, ResultsWarning: The NCBI website requires JavaScript to operate. Bath of Body Fat With C-Reactive Protein in Rheumatoid ArthritisJon T. Giles1 Jon T. Giles, MD, Susan J. Bartlett, PhD, Richard Thompson, PhD, Kevin R. Fontaine, PhD, Joan M. Bathon, MD. The concentration of reactive proteins of serum C (CRP) is commonly used in rheumatoid arthritis (RA) as a subdued marker of systemic inflammation, presumably induced by synovitis. However, other tissues, such as adipose tissue, can induce CRP production. This study was conducted to explore partnerships between adiposity measures and CRP levels in the RA. MethodsOne hundred and ninety-six men and women with RA were subjected to anthropometric evaluation and total absorption of double-body X-ray for the measurement of total and regional body fat and magra mass. The associations between magra mass measures and mass and serum levels of CRP and interleukin-6 (IL-6) were determined in sex-strateged analysis, with adjustment to covariate the relevant demographic disease and treatment, and for the possible effects of modification of joint activity and pharmacotherapeutic biologic agents. ResultsAll adiposity measures were significantly associated with the level of CRP in women, but not in men. In women, the measure of adiposity shown by the strongest association with the level of CRP was truncaline fat, in which, in adjusted analysis, each increase of kilogram was associated with an increase of 0.101 units in the level of CRP transformed logarithmically (P ConclusionAdiposity is associated independently with CRP levels in women with RA, and therefore can confuse the estimated seramic activity In rheumatoid arthritis (RA), the level of CRP is frequently used in conjunction with evaluations of joint inflammation and tenderness to estimate the level of activity of the disease and, in addition to the erythrocyte sedimentation rate, is a component of the nucleus of the American College of Rheumatology established to measure the clinical response in the RAmark trials (), is a component of the activity of the disease in 28 ha. CRP is a 23 kd subunits pentamer that is synthesized and secreted by hepatocytes when stimulated by a variety of inflammatory cytokines, including the tumor necrosis factor α (TNFα), interleukin-1 (IL-1), and especially IL-6 (). Under these conditions, serum CRP levels can increase ≥100 times more than baselines (). In addition to being a sensitive surrogate of the response in the acute phase, a growing level of CRP may also have direct pro-inflammatory effects, including the activation of supplement and induction of the tissue factor (). In the RA, the inflated synovium and the circulating monocytes are sources of cytokines that induce the production of CRP. However, other tissues are known sources of these cytokines. The adipose tissue is a powerful source of inflammatory cytokines, including TNFα and IL-6, which induce the liver production of CRP. In studies of the general population, an association between body fat mass and circulating CRP levels has been confirmed (). In particular, the visceral adipose tissue, distributed within the intraabdominal cavity and surrounding the mesentry and omento, has been shown to be the adipose deposit with the greatest contribution to systemic inflammation (). Interventions that reduce the mass of adipose tissue (e.g. weight loss) are associated with a decrease in the production of CRP (). To investigate the possible contribution of adiposity to the CRP levels in the RA, we compare relative contributions of anthropometric and dual-energy x-ray absorptiometry (DXA) – derivative body fat measures, along with features of the RA disease, demographic and lifestyle factors and cardiovascular risk factors, to the concentration of CRP serum in men and women with RA. We also investigate whether the levels of swelling and joint tenderness modified the association between body fat and CRP. PATIENTS AND METHODS The topics were participants in the ESCAP trial (Assessment of subclinical cardiovascular disease and event predictors in rheumatoid arthritis), a cohort study that investigates the prevalence, progression and risk factors of subclinical cardiovascular diseases in the RA. Topics were included if they met the classification criteria of the American College of Rheumatology (formerly the American Rheumatism Association) 1987 for the RA () and were 45 to 84 years. Subjects were excluded if they reported any cardiovascular event diagnosed by the doctor prior to registration, including myocardial infarction, congestive heart failure, coronary bypass graft, angioplasty (with or without arterial placement), peripheral vascular disease or peripheral arterial vascular procedures, implanted pacemakers or defibrillators, and current atrial fibrillation. The subjects weighing more than 300 pounds were also excluded due to the weight limitations of the cardiovascular imaging equipment used in the study. ESCAP participants were recruited from patients who were followed at the Johns Hopkins Arthritis Center, and by referral of local rheumatologists. The study was approved by the Johns Hopkins Hospital Institutional Review Board, with all subjects providing written consent prior to registration. The registration began in October 2004 and ended in May 2006. EvaluationsComposition of bodies Subjects undergoing a total analysis of the DXA body in a Lunar Prodigy DXA scanner (GE/Lunar Radiation, Madison, WI), with results analyzed using Prodigy software (version 05.60.003). DXA was used to analyze and measure body fat, lean mass and bone mass in the total body (less the head) and by region of the body (armas, legs and trunk). The automated quantification of the total and regional masses of body tissue, using the validated software of the manufacturer, was in real time, with the entire process of acquisition and analysis carried out by the scanner and the technician at the time of the exploration of topics. Each subject was scanned on the same DXA scanner, and the quality control and calibration procedures were performed daily according to the standard protocol provided by the manufacturer. All subjects were subjected to height measurements (in cm) and weight (in kg) with a wall mounted stage and a Detecto scale, respectively, with the subject placed in a standing position and with light underwear and without shoes. The body mass index (BMI) was calculated as body weight (in kg) divided by height (in m2). The waist and hip circumferences were measured with a Gulick II anthropometric tape, using a standard protocol. The circumference of the waist was measured at the umbilicus level, and the circumference of the hip was measured at the maximum circumference of the buttocks. Other features The demographic, lifestyle and RA disease characteristics were evaluated on the same day as the evaluation of body composition. Each of these characteristics was determined by trained examiners using a structured interview in formalized questionnaires. A single trained evaluator examined 44 joints for swelling, tenderness, deformity and surgical replacement or fusion. The duration of the RA was evaluated by the patient self-reportation from the date of diagnosis. The severity of the RA was estimated using the sum of the number of joints exhibiting deformity or requiring surgical substitution/fusion (). The activity of the RA disease was calculated using DAS28 with the measurement of the CRP included (). For analysis with CRP as a dependent variable, the activity of the disease was estimated using the swollen joint count or the sum of the swollen joint count and the counting of tender joints (more tender swollen joints). Functional limitation was evaluated with the Stanford (HAQ) health assessment questionnaire (), modified to include a subcategory score for those who reported that they needed assistance from others or use aid devices. Current use and past use of biologic and non-biological (DMARD) glucocorticoids and antireumatic drugs were determined by detailed questionnaires and administered by the examiner. The subjects were classified as current smokers if they reported a current smoking habit and the total number of smoked cigarettes in their lives was at least 100. Physical activity was evaluated using the 7-day Physical Activity Recall questionnaire (). Subjects were classified as regular assets if the average daily average of the total weekly self-reported physical activity for intentional exercise activities (moderate or fast-risk payrolls for exercise, and individual sports and fitness or moderate or vigorous equipment) amounted to ≥30 minutes per day ≥5 days per week, in accordance with current recommendations for physical activity (). In addition, the subjects reported the duration of daily television, a sedentary activity measure. Subjects were classified as diabetes if the level of blood fasting glucose was ≥126 mg/dl or were taking diabetes medications. Subjects were classified as dyslipidemia if the concentration of high-density lipoprotein serum (HDL) of cholesterol was 150 mg/dL, or if the subject was taking medications that decreased lipids. The level of CRP was determined with a method of high-sensitivity nephelometry (Dade Behring, Deerfield, IL-6), and IL-6 was determined by the enzyme-related immunosorbent (ELISA) (R pestD Systems, Minneapolis, MN) at the Clinical Biochemistry Research Laboratory (University of Vermont, Burlington, VT). The level of serum glucose was measured by spectrophotometry of rate reflectance, HDL cholesterol levels were measured using the method of cholesterol oxidation (diagnosis of the time, Laval, Quebec, Canada) and triglycerides levels were determined using the Triglyceride GB reagent (diagnosis of the time) at the University Clinical Laboratory of Fair Studies. The presence of the rheumatoid factor (RF) was evaluated using ELISA, in the clinical laboratory of the Johns Hopkins Hospital (Baltimore, MD), with RF seropositive defined as ≥40 units. Statistical Analysis In groups stratified by sex, continuous variables were compared using the unpainted t test, with results expressed as the mean ± SD. For the comparison of variables not normally distributed, the Kruskal-Wallis test was used, with the results expressed as the mean and interquartile range. For categorical variables (counts and percentages of swollen and tender joints), the results were compared using the relatively small benefit goodness test or Fisher's exact test, as appropriate. Simple models of linear regression were built to explore the univariated partnerships between the log CRP (i.e., the CRP level transformed logarithmically to normality using natural registration) and the demographic, lifestyle, RA disease and body composition characteristics of subjects, in sex-stricken analysis. The height adjustment was performed in all regression analysis involving lean or fat mass, either total or truncale. Since truncale fat was determined to be the body composition component with the largest association with CRP log, the truncale fat mass was retained as the independent variable of interest in the subsequent multivariate modeling. Multivariate linear regression models were used to further explore the association between the CRP log and the truncale fat mass, with adjustments to the demographic characteristics and the relevant RA disease. A simple model (model 1) was built using only variables that were significantly associated with the dependent variable in univariated comparisons. A second model (model 2) was built using the independent interest variable (fecal fat) adjusted only for demographic, RA disease and treatment characteristics. A third model (model 3) included a new adjustment for lifestyle characteristics, cardiovascular risk factors, physical activity and menopause (only in women). The total variability in the registry CRP explained by the model variables was estimated using the determination coefficient (R2). To corroborate the observed results, the analysis was repeated using the IL-6 instead of the CRP as a dependent variable, in analysis using the same protocols described above. We then investigate whether the CRP association with truncale fat differs depending on the level of activity of the disease. Because the CRP is a basic component of the DAS index, swollen joint counts or the sum of tenderer swollen joint counts were used as alternative definitions of disease activity. The swollen joint counts and the tenderest swollen joint counts were plotted against the CRP log to determine the level of activity of the joint disease in which a significant association was obtained with the CRP, giving cutting values (by activity of "high" versus "low" joint disease, both in men and in women in this sample) of 10 swollen joints and 16 more tender swollen joints. Statistical interaction models were built to assess whether high levels of swollen joints or more tender swollen joints significantly modified the trincal trunk-grase ratio, in sex-strateged analysis. Similar interaction models were built according to the current use of biological DMARDs. Statistical calculations were performed using Stata 9 (StataCorp, College Station, TX). In all tests, a α value of 2 tails of 0.05 was defined as the level of statistical significance. RESULTS Comparison of the characteristics of subjects by sex Ninety-six subjects were studied (118 women and 78 men). The characteristics of the themes at the base are summarized in . Compared to male subjects, female subjects had significantly higher joints, tender joints, HAQ scores and total deformity. The average levels of CRP do not differ significantly between sexes. More female subjects than male subjects received treatment with biological DMARDs; however, the current use of non-biological glucocorticoids and DMARDs does not differ by sex. Although the mean BMI and the distribution of topics between the 3 categories of BMI do not differ by sex, female subjects had a significantly higher total fat mass and a significantly higher percentage of body fat compared to male subjects. Despite these differences, the truncale fat mass does not differ significantly between the sexes. 0 Characteristics of subjects of study*Characteristics (n = 78)Women (n = 118) Demographic age, mean ± SD years59.3 ± 9.959.5 ± 7.80.90 Caucasian69 (88.5)101 (85.6)0.73 Current smoke13 (16.7)10 (8.5)0.087 Diabetes7±0±0 Among the male subjects, significant univariated partnerships with CRP log were observed during the growing age, the increasing duration of the RA, the highest joint counts and the greatest joint total deformity. In addition, it was observed that the current use of biological DMARDs had a significant negative association with CRP log in men. However, no measure of body composition was significantly associated with CRP log in men. Table 2Univariated regression ratios for CRP log associations with clinical and demographic characteristics between male and female subjects* MaleFemaleCharacteristicβPR2βPR2Demographic Age0.0370.0170.073−0.002NS Among female subjects, the only demographic characteristic significantly associated with the logistic CRP was Caucasian race, in which there was an average difference of 2.06 mg/liter In women, no characteristic of RA disease or treatment characteristic was significantly associated, either positive or negative, with the registry CRP. On the contrary, all the adiposity measures were closely associated with the CRP of registration in women, with a truncale fat that demonstrated the greatest magnitude of the association. Unlike male subjects, it was observed that women had significant associations between physical activity factors and CRP log, more often than regular exercise that had a negative association with the result and increased sedentary activity that had a positive association with the result. The results of the multivariate models that explore the associations between the truncale fat mass and the CRP log are summarized in (listed only for women, as no adiposity measure was significantly associated with CRP levels in men). In the simplest model (model 1), which was adjusted only for covariates that showed significant univariated partnerships with CRP log, each increase in mass kg of truncacal fat was associated with an increase of 0.098 units in the CRP log (P Table 3Multi-annual regression ratios for CRP log associations with clinical and demographic characteristics among female subjects* Model 1Model 2†Model 3‡Variableβ PβPβPTruncal mass fat0.098 There were few changes in the magnitude of the association of the truncale fat mass with the CRP log in the fully adjusted model (model 3), which included the same covariates adjusted for model 2 along with the menopausal state, cardiovascular risk factors and physical activity, with each kilogram increase of the mass None of the demographic, lifestyle or disease or treatment characteristics of the RA, including swollen or tender joint counts, were significantly associated with the CRP of the trunk after adjustment. Although the truncale fat mass was the measure of adiposity with the greatest magnitude of the association with CRP log in women, other adiposity measures were also found independently associated with CRP log. The substitution of the BMI for truncale fat mass in multivariate model 3 revealed that each increase in the BMI unit was associated with an increase of 0.084 units in the CRP log (P = 0.001). By using other similar substitutions in models fully adjusted in women, we find that each 1-cm increase in the waist circumference was associated with an increase of 0.027 units in the CRP registry (Replacement P of the log IL-6 for the log CRP produced similar relationships, both in men with RA and in women with RA (no data is shown). Interaction of joint symptoms in the truncale-CRP ratio In swollen joint-recount stratified models (≥10 swollen joints versus minimal squares linear regression analysis of the interaction of the more tender swollen joint levels in the relationship between the C-reactive protein level (Ln CRP) and truncacal fat in women with rheumatoid arthritis. Broken lines indicate the confidence intervals of 95% of the estimates. The female subjects are divided according to the level of swollen joints more tender, with joint activity "high" (in solid line) and "low" joint activity (tonalized line), defined as a more tender swollen joint count of ≥16 and In contrast, in men, the relationship between truncacal fat and the CRP of trunk differs by level of joint activity (). A significant negative linear relationship was observed between truncale fat and CRP log in men with high counts of swollen joints, with each kilogram of increase of truncaline fat associated with a decrease of 0.171-unity in CRP log in men in this group (P for interaction = 0.004) compared to no significant relationship between truncacal fat and CRP log in men with lower levels of inflammation = 0.00r6). Similar results were observed in men stratified by higher counts of tenderer swollen joints (). Linear regression analysis of minimal squares of the interaction of the more tender swollen joint levels in the relationship between the level of C-reactive proteins (ln CRP) and truncaline fat in men with rheumatoid arthritis. Broken lines indicate the confidence intervals of 95% of the estimates. Male subjects are divided according to the level of swollen joints more tender, with joint activity "high" (in solid line) and "low" joint activity (tonalized line) defined as a more tenderly swollen joint count of ≥16 and interaction of use of biological DMARD in the truncated fat ratio Relationships were not modified by the level of joint activity or by the use of biological DMARDs in women. On the other hand, a significant relationship was observed between truncale fat and CRP levels in men with high counts of more tender swollen joints. However, this relationship was the opposite of the one observed in women, as the men of this subgroup had increased trucal fat in association with a decreasing CRP level. Similar findings were shown when IL-6 levels were used as a substitute for CRP levels, suggesting that the observed effects can be mediated by the production of IL-6 with adipose origin. In a recent report (), investigators identified an association between waist circumference and CRP levels in RA patients. Our study differs from this previous study in which we use direct quantification, by DXA, of total body fat mass and regional body fat mass, and use a larger sample of RA patients, which facilitated the detection of sex differences in the adiposity-CRP association. These results suggest that body fat, in particular truncale fat, should be considered when interpreting the importance of a high level of CRP in women with RA, and imply that a fat-associated elevation in CRP may confuse clinical diagnosis and therapeutic decision-making in a variety of configurations. For example, when using the sérico CRP concentration as a diagnostic tool, a fat-associated elevation in the CRP in a woman with non-inflammatory musculoskeletal symptoms could cause an inaccurate diagnosis of seronegative RA. In other contexts, such as the use of the serum CRP concentration to guide therapeutic decision-making, a fat-associated elevation in the CRP can be misinterpreted as a reflection of the persistent synovitis. Ironically, obesity can make the joint examination, and therefore the exact evaluation of the synovitis, difficult, and the CRP level can be more easily based on measuring the activity of the RA disease. Thus, a fat-associated elevation at the CRP level can boost the practitioner to unnecessarily accelerate immunomodular therapy. In clinical trials, the effectiveness of a pharmacotherapeutic agent could be underestimated when the CRP concentration is used as part of the effectiveness result measure. In fact, it has been suggested that women have lower response rates to treatment despite similar levels of joint symptoms (,). Inflammation associated with fat can be, at least in part, a source of this sexual discrepancy. Our study identified striking sexual differences in the relationship between body fat and CRP levels. The basis of these differences is not immediately evident, but could involve several possibilities. First, the influence of hormones could modify the association, as an inverse relationship between testosterone and CRP levels has been reported. Estrogen deficiency, such as polycystic ovary syndrome, has also been associated with high levels of CRP, independent of a fat association (). Another reason for sexual differences could be the ability to detect the inflammatory potential of adiposity deposits. Although all the fatty tissue has been involved in inflammatory cytokine production, visceral fat seems to have the greatest potential to express cytokines that induce liver expression CRP (). Both subcutaneous and visceral fats are quantified by DXA and the truncale fat mass. Therefore, it is possible that the use of methods that specifically measure visceral fat (i.e., abdominal computed tomography) allows the detection of a relationship between visceral fat and CRP level in men. However, other gender differences have been observed in predictors of a high level of CRP, suggesting fundamental differences between men and women in CRP induction mechanisms. Predictors of an elevated CRP level that are characteristics of the RA disease process (for example, duration of disease or swollen joint counts) were seen in men, whereas in women, measures of RA disease and gravity were not as robustly associated with the CRP level, despite many of these predictors being generally more prevalent in women. On the basis of these fundamental differences, we explore the possibility that the associations observed between the fat mass and the CRP were modified by the level of activity of the RA disease, with the hypothesis that as the level of the swollen and tender joints increased, the influence of the fat mass at the CRP level would be flooded. This was not the case in women, in which there was no significant difference in the association between the CRP and trucal fat mass between women with low levels of swollen and tender joints and women with high levels of swollen and tender joints, highlighting the profound influence of adiposity on the CRP levels in women at all levels of joint activity. The level of joint activity of the RA changed the relationship between truncale fat and the CRP level in men, with the increase of the trucal fat mass associated with the decrease in CRP levels in men with high swollen and tender counts. This finding was unexpected and not easily explanatory, but highlights, in previously unexplored ways, the potential of body fat to influence the dynamics of the CRP expression in RA patients. High levels of joint inflammation in men with high disease activity may overwhelm the effects of inflammation associated with fat at systemic CRP levels, or that joint inflammation may directly or indirectly inhibit the production of inflammatory cytokines by adipose tissue in men. It will be of interest to confirm this partnership in additional populations. We also seek to explore whether the use of biological DMARDs, with its deep ability to suppress the production of sworn inflammatory citochines, could also modify the association of adiposity with the level of CRP. We do not find any modification of the effect of biological agents on men or women, suggesting that biological therapies may not have an effect on the suppression of inflammatory cytokines in the adipose tissue in RA patients. This finding contrasts with that obtained in previous short-term intervention studies (in non-ARA cohorts), in which it was shown that a TNF inhibitor (tanercept) could suppress the systemic levels of CRP in obese patients with metabolic syndrome or type 2 diabetes (,). The discrepancy between our findings and previous studies could be a by-product of our cross-sectional design, as the association between adiposity and the level of CRP might have differed between patients treated with TNF inhibitor and not treated before starting biological therapy, but with the prolonged use of TNF inhibitor, the strength of the association could have matched. Another possibility is that RA and non-RR populations differ in terms of the ability of TNF inhibitors to suppress fat-associated inflammation, perhaps related to prolonged exposure to the biological agent. Curiously, other studies have identified side effects of TNF inhibitors at metabolic endpoints (), suggesting that compensatory mechanisms may annul the beneficial effect of TNF inhibition on extra-articular tissues, in conditions of prolonged exposure to these agents. The CRP is not directly expressed by adipose tissue, but its synthesis in the liver is induced by a series of cytokines of adipose origin, mainly IL-6 (). We seek to confirm the possible intermediate effect of IL-6 at the CRP level by exploring the fat mass association with IL-6 serum levels. The finding that the relationships between fat mass and IL-6 levels were similar to those between fat mass and CRP levels suggests that IL-6 is a mediator of the fat mass association-CRP. Other adipose cytokines, such as TNFα, are difficult to measure in patients receiving TNF inhibitors. The analysis of the hormones derived from adiposease, such as leptin and adiponectin, could also reveal links between the fat mass and the CRP level in patients with the RA (), and a new research of these associations is being carried out. We do not identify any relationship between lean mass measures and CRP levels, either in men with RA or in women with RA. Previous studies in RA patients have observed low body mass associations with high levels of TNFα induced in peripheral blood monocytes (,). A study identified a simple low lean mass correlation with the CRP level (); however, the potential confusing effects of body fat at the CRP level were not considered in that study. In our study, the truncale fat mass quantified by the total DXA body was the measure of adiposity with the highest degree of association with the CRP level. However, it was found that other adiposity measures with high correlations to truncaline fat (i.e. waist circumference, total fat mass and BMI) were also significantly associated with the CRP level. In the absence of DXA scanning, which may not be feasible for all patients in clinical practice, the practitioner may use waist circumference or BMI as a reasonable proxy for truncaline fat to estimate the contribution of truncaline fat to systemic inflammation. The additional limitations of the current investigation must be recognized. The subjects were participants in a study that excluded patients whose weight exceeded 300 pounds and/or patients who had a history of cardiovascular disease. Based on the identification of links between adiposity, CRP level and cardiovascular disease (,), patients with the most robust adiposity-level partnerships between CRP may have been excluded. However, the inclusion of these topics is likely to strengthen, not reduce, the magnitude of the partnership observed between adiposity and the level of CRP. In addition, the cross-sectional design of our study limits the ability to attribute causal relationships to the detected associations. However, because there is no biologically tenable hypothesis to indicate that the elevations at the CRP level induce the acquisition of runcal fat, it is more likely that runcal fat will induce an elevation at the CRP level. If this effect occurs directly through dynamized IL-6 or occurs through other mechanisms it cannot be systematically established through our study. In short, we show a strong association between body fat, in particular truncale fat, and the CRP serum concentration in women with RA. Neither the level of joint activity nor the use of biological DMARDs modified the association. Men with RA did not exhibit the same association of body fat with the CRP level, suggesting that there is a fundamental difference related to sex in the interaction between body fat and induction CRP that justifies an additional research. These findings suggest that body fat can confuse commonly attributed associations between factors related to RA disease and serum CRP concentration in certain patients, and body fat should be considered when using the CRP level for diagnostic and therapeutic decision-making in RA patients. Acknowledgements Partly supported by NIH grants (National Institute of Arthritis and Musculoskeletal and Skiing Diseases AR-050026-01 and 1K23-AR-054112-01) and the Johns Hopkins Bayview Medical Center General Clinical Research. Dr's work. Giles was also supported by a grant from clinical researchers at the American College of Rheumatology Research and Education Foundation. We would like to thank the staff of the Johns Hopkins Bayview Medical Center for Clinical Research for supporting the DXA scan used in this study. We are also indebted to the staff of ESCAP (Cities of Mary, Michelle Jones, Patricia Jones, Marissa Hildebrandt and Shawn Franckowiak) for their dedication and hard work. Besides, we'd like to thank Dr. Uzma Haque, Clifton Bingham III, Carol Ziminski, Jill Ratain, Ira Fine, Joyce Kopicky-Burd, David McGinnis, Achini Perera, Peter Holt, Megan Clowse, and Gordon Lam, among others, for generously recommending their patients for this study. Footnotes. Bathon has received consulting fees, speech fees and/or fees from Abbott, Amgen and Centocor (less than $10,000 each) and research support from Amgen, Biogen Idec and Bristol-Myers Squibb. AUTOR CONTRIBUTIONSDr. Giles had full access to all the data in the study and was responsible for the integrity of the data and the accuracy of the data analysis. Studio design. Giles, Bathon. Data acquisition. Giles, Bathon. Analysis and interpretation of data. Giles, Thompson, Bathon. Preparation of manuscripts. Giles, Bartlett, Andersen, Fontaine, Bathon. Statistical analysis. Giles, Thompson.ReferencesFormats: Share , 8600 Rockville Pike, Bethesda MD, 20894 USA

What Is C-Reactive Protein? What It Can Tell You About Your Autoimmune Disease – CreakyJoints

Identifying patients with rheumatoid arthritis with moderate disease activity at risk of significant radiographic progression despite methotrexate treatment | RMD Open

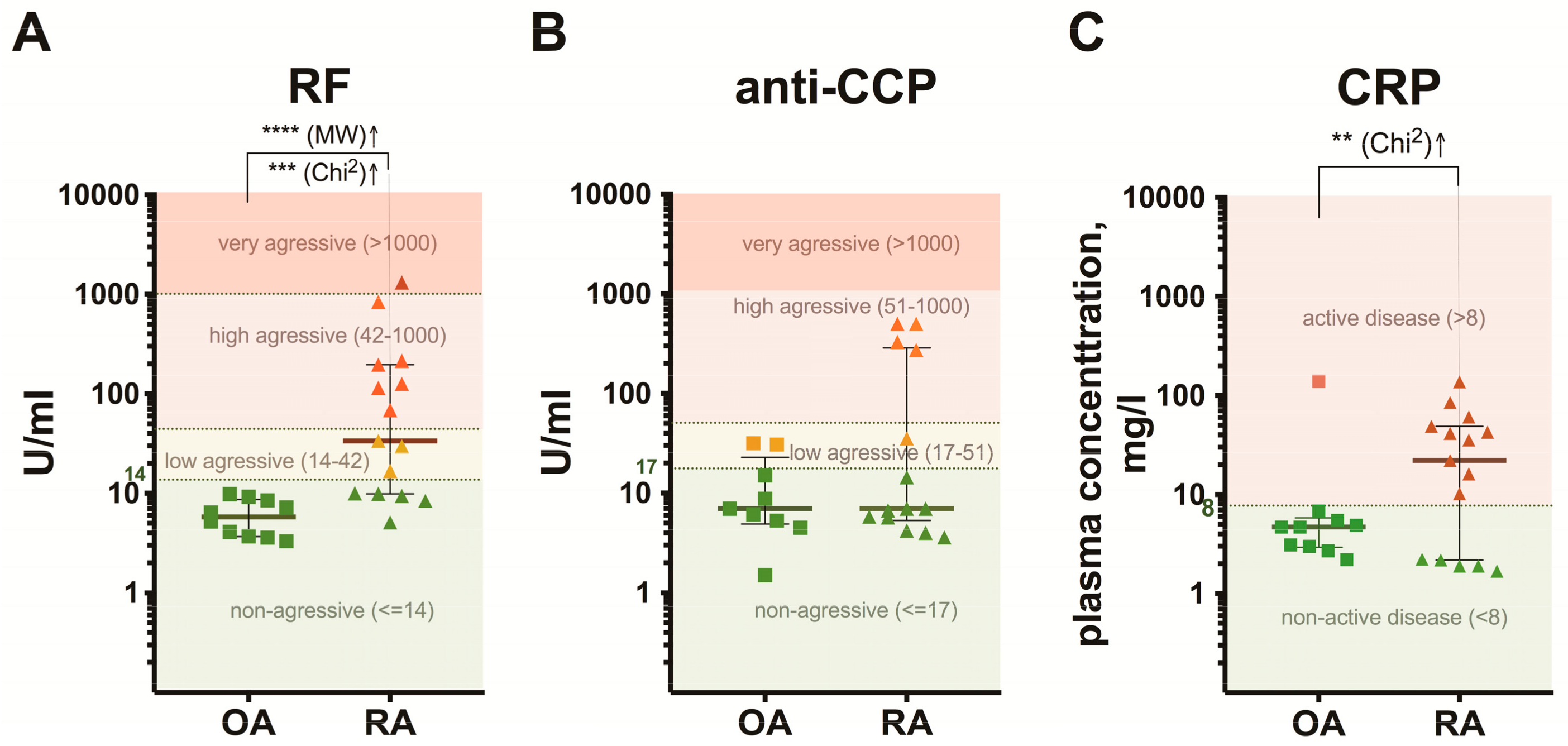
Infliximab rapidly normalizes C-reactive protein levels in rheumatoid... | Download Scientific Diagram
PLOS ONE: Levels of C-Reactive Protein Associated with High and Very High Cardiovascular Risk Are Prevalent in Patients with Rheumatoid Arthritis
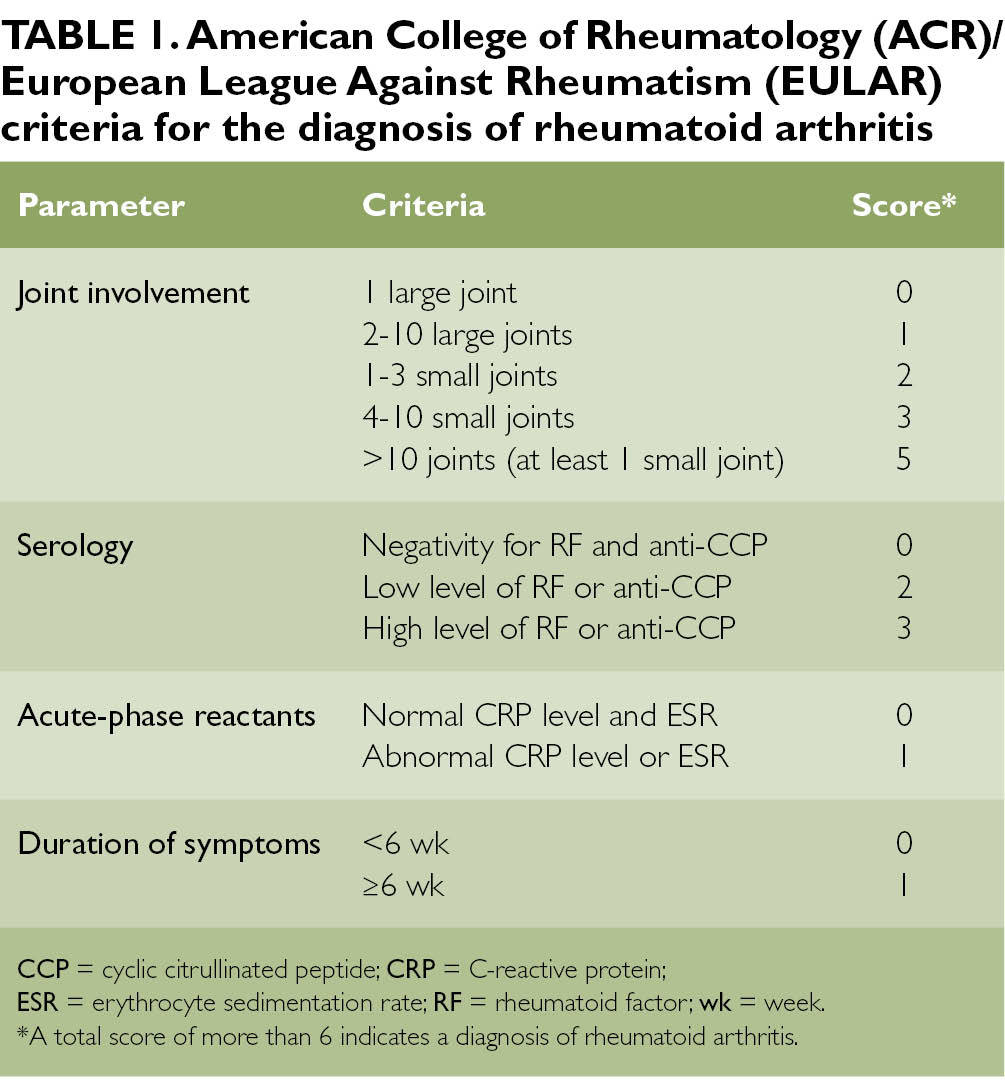
Rheumatoid arthritis: risk factors, clinical signs, and treatment - Page 2 of 3 - Clinical Advisor
![rheumatoid_arthritis [TUSOM | Pharmwiki] rheumatoid_arthritis [TUSOM | Pharmwiki]](https://tmedweb.tulane.edu/pharmwiki/lib/exe/fetch.php/raeffects.png)
rheumatoid_arthritis [TUSOM | Pharmwiki]

Hemoglobin Level, ESR, platelet count, RF and CRP in rheumatoid... | Download Table

C-Reactive Protein (CRP) Test: Normal and High levels, Treatment
Rheumatoid arthritis
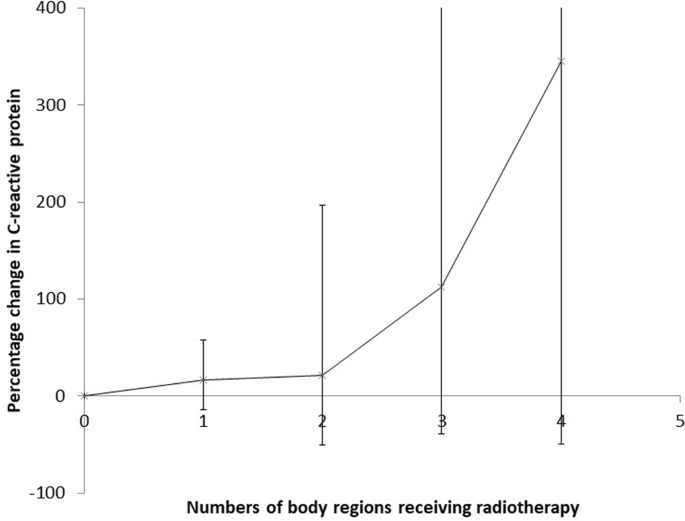
Inflammatory disease and C-reactive protein in relation to therapeutic ionising radiation exposure in the US Radiologic Technologists | Scientific Reports
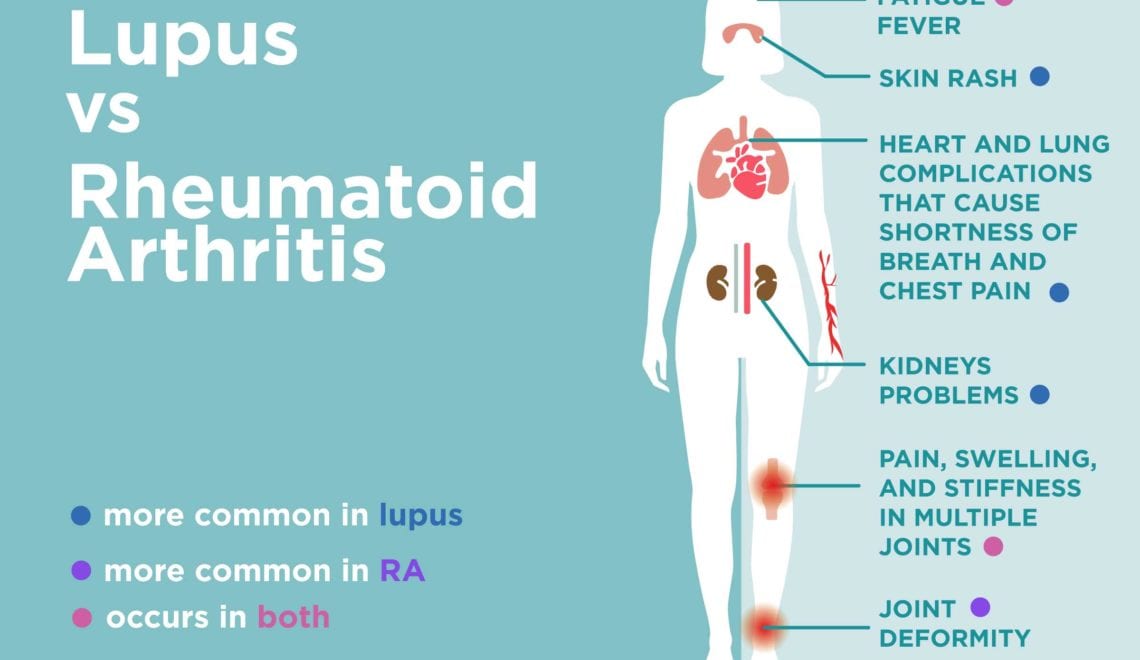
Lupus vs. Rheumatoid Arthritis: What's the Difference? – CreakyJoints

Rheumatoid Arthritis and Osteoarthritis: How to Assess Patients (Page 2)
![PDF] Erythrocyte Sedimentation Rate and C-reactive Protein Measurements and Their Relevance in Clinical Medicine. | Semantic Scholar PDF] Erythrocyte Sedimentation Rate and C-reactive Protein Measurements and Their Relevance in Clinical Medicine. | Semantic Scholar](https://d3i71xaburhd42.cloudfront.net/6e3479f7ece84338948a67874038bc592f057424/4-Table2-1.png)
PDF] Erythrocyte Sedimentation Rate and C-reactive Protein Measurements and Their Relevance in Clinical Medicine. | Semantic Scholar

Schematic time course of C-reactive protein levels and concurrent... | Download Scientific Diagram

xmlinkhub

Increased C reactive protein in response to acute stress in patients with rheumatoid arthritis | Annals of the Rheumatic Diseases

CRP and Inflammation – This Blog Post Could Save Your Life | Thorne
Medicina | Free Full-Text | Proportion of the CD19-Positive and CD19-Negative Lymphocytes and Monocytes within the Peripheral Blood Mononuclear Cell Set Is Characteristic for Rheumatoid Arthritis | HTML

View Image
Personalized Medicine in RA: The Role of Biomarkers (Transcript)
PLOS ONE: Paradoxical Association of C-Reactive Protein with Endothelial Function in Rheumatoid Arthritis
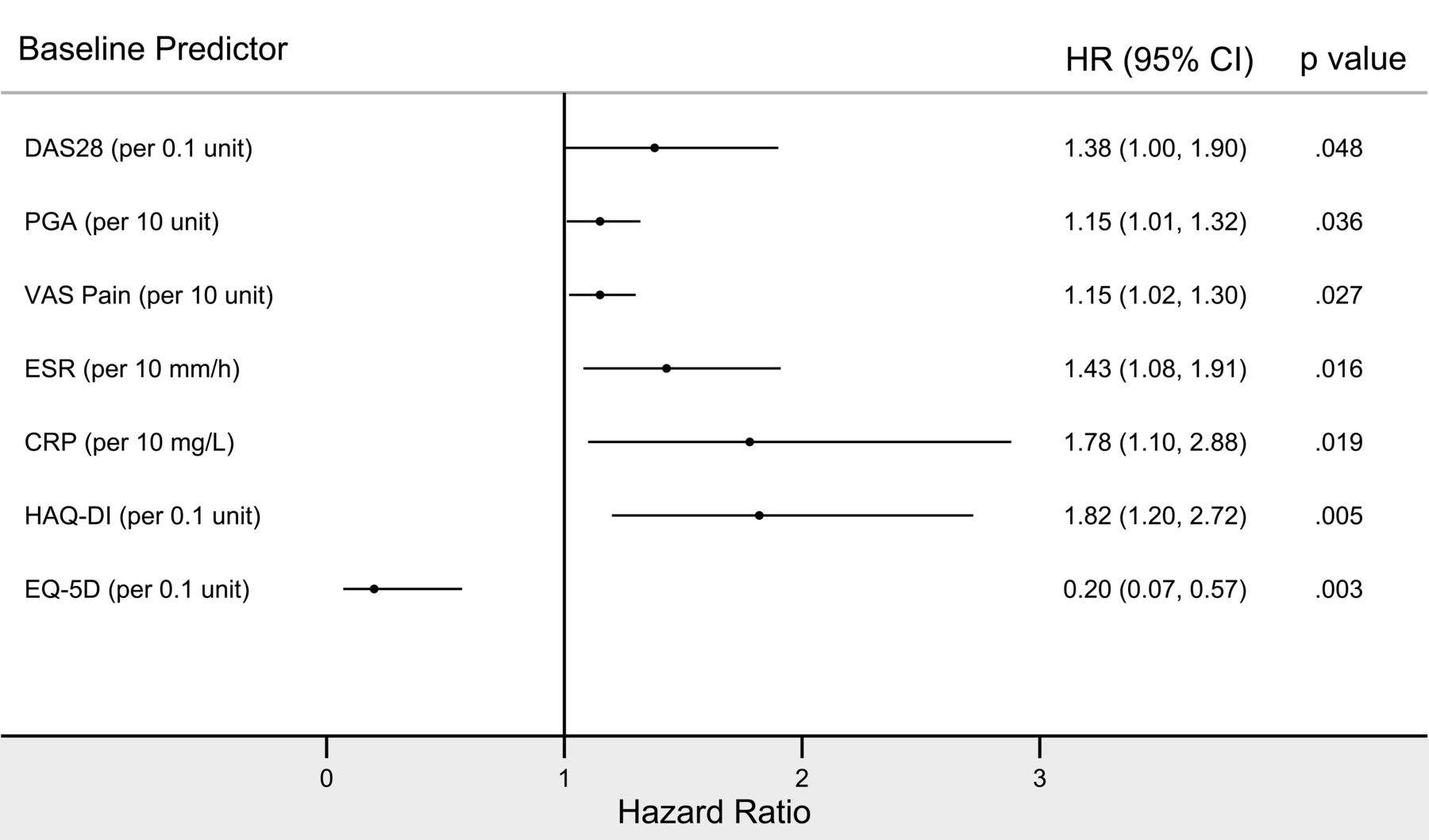
Flares in Rheumatoid Arthritis Patients with Low Disease Activity: Predictability and Association with Worse Clinical Outcomes | The Journal of Rheumatology

Rheumatoid Arthritis and Osteoarthritis: How to Assess Patients (Page 2)
Rheumatoid Arthritis (RA) Tests | Diagnosing & Testing for RA

C-reactive protein (CRP) test: High levels, low levels, and normal range

Atherogenic lipid profile and high sensitive C-reactive protein in patients with rheumatoid arthritis. | Semantic Scholar
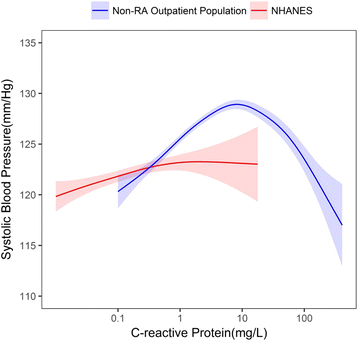
Association between inflammation and systolic blood pressure in RA compared to patients without RA | Arthritis Research & Therapy | Full Text
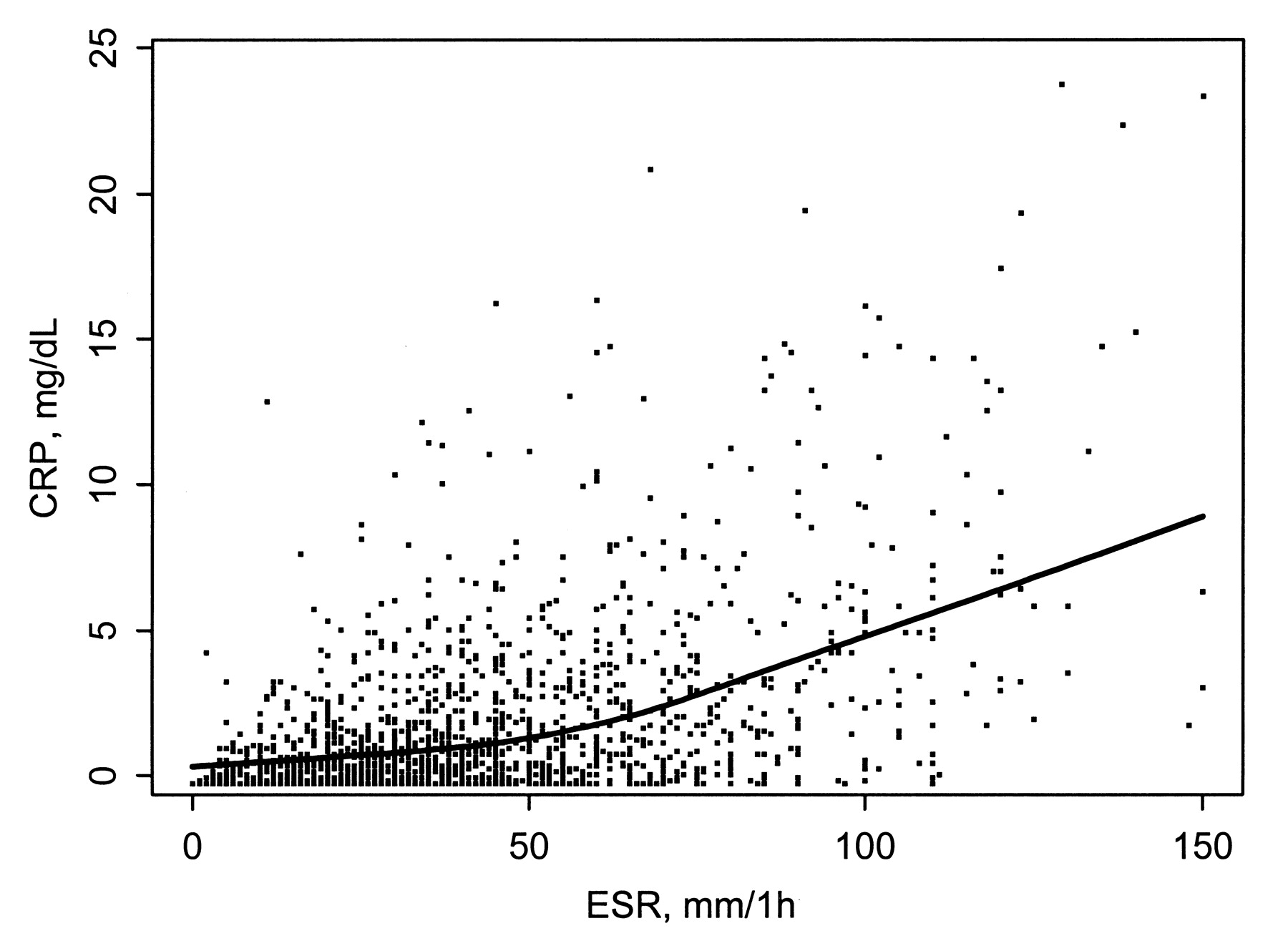
Which Measure of Inflammation to Use? A Comparison of Erythrocyte Sedimentation Rate and C-Reactive Protein Measurements from Randomized Clinical Trials of Golimumab in Rheumatoid Arthritis | The Journal of Rheumatology

C-Reactive Protein and Coronary Artery Calcium in Asymptomatic Women With Systemic Lupus Erythematosus or Rheumatoid Arthritis - American Journal of Cardiology
PLOS ONE: Circulating Protein Fragments of Cartilage and Connective Tissue Degradation Are Diagnostic and Prognostic Markers of Rheumatoid Arthritis and Ankylosing Spondylitis

Exemptia Rheumatoid Arthritis Blood Test C reactive protein CRP is a protein synthesized by liver when there is inflammation infection in the body Usually done to measure the amount of CRP protein

Abbreviations: CDAI Clinical Disease Activity Index, CRP C-reactive... | Download Scientific Diagram
Acupuncture And Herbs Quell Rheumatoid Arthritis

Central Pain in Rheumatoid Arthritis

Correlation of C-reactive protein haplotypes with serum C-reactive protein level and response to anti-tumor necrosis factor therapy in UK rheumatoid arthritis patients: results from the Biologics in Rheumatoid Arthritis Genetics and Genomics

View Image
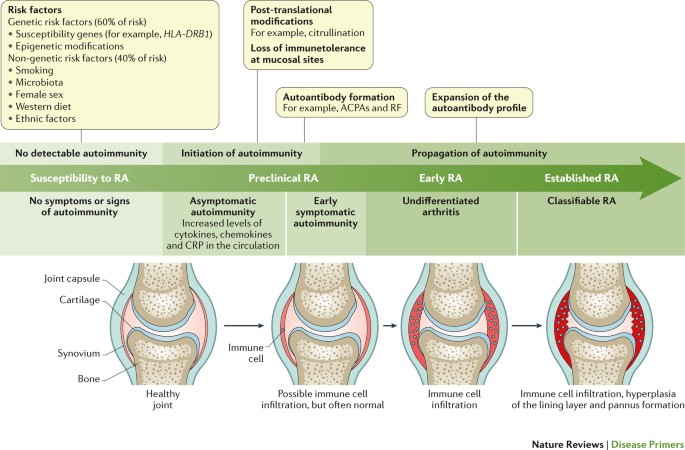
Rheumatoid arthritis | Nature Reviews Disease Primers

Exemptia Rheumatoid Arthritis Blood Test C reactive protein CRP is a blood test marker for inflammation in the body which is produced in the liver The level of CRP can be measured

Impact of certolizumab pegol on patient-reported outcomes in rheumatoid arthritis and correlation with clinical measures of disease activity | Arthritis Research & Therapy | Full Text
:max_bytes(150000):strip_icc()/what-is-rheumatoid-factor-190280-c0a3fb6a38da458bb3152e17efb82cd0.png)
Rheumatoid Factor Blood Test: Uses, Procedure, Results
Posting Komentar untuk "c reactive protein rheumatoid arthritis"